Hospitals and health systems nationwide face increasingly tight operating margins as persistently high expenses take their toll, driven by inflation, long-running workforce shortages, and other economic forces. Navigating continued volatility requires healthcare leaders to take a comprehensive approach to cost reduction strategies that will help contain costs long-term.
Organizations need to assess current, ongoing performance improvement plans to determine their effectiveness and make adjustments to close financial gaps. Creating viable and robust strategies to build financial stability requires an understanding of costs related to supplies, labor, and clinical performance, and integration across your organization to set realistic targets for each of those areas.
These four strategies can help your organization create an enterprise performance management (EPM) infrastructure to achieve your cost-reduction goals:
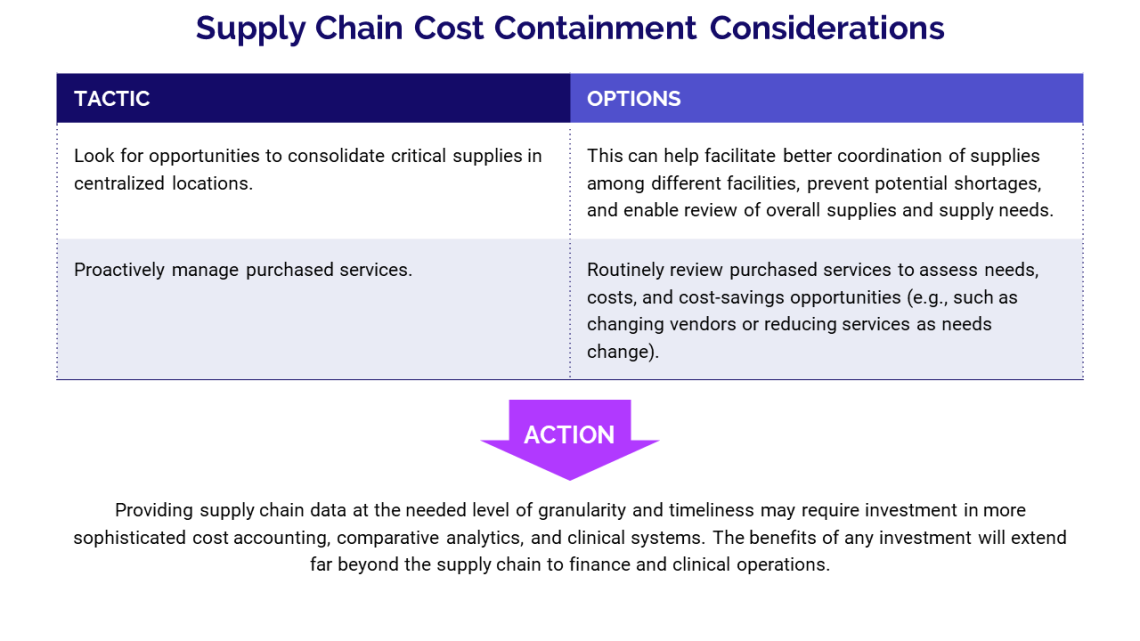
Strategy 1: Compare supply chain costs to detect variations
Hospitals and health systems depend on their supply chain to manage what can account for as much as 40% of an organization’s costs. The supply chain must establish processes that make it easy to link purchased products and services to individual patient encounters.
Cost and utilization data enable supply chain leaders to detect variations across departments and facilities, identify areas where product standardization could generate savings, support bundled-payment and pricing initiatives, and provide greater leverage for volume-based discounts from vendors. Utilization data can support predictive modeling for demand trends to ensure sufficient inventory.
Supply chain leaders need to benchmark their performance, both internally and against peer organizations, to put their performance in context and identify opportunities for improvement. Where the supply chain excels, comparative analysis can validate and quantify the supply chain’s contributions to the organization.
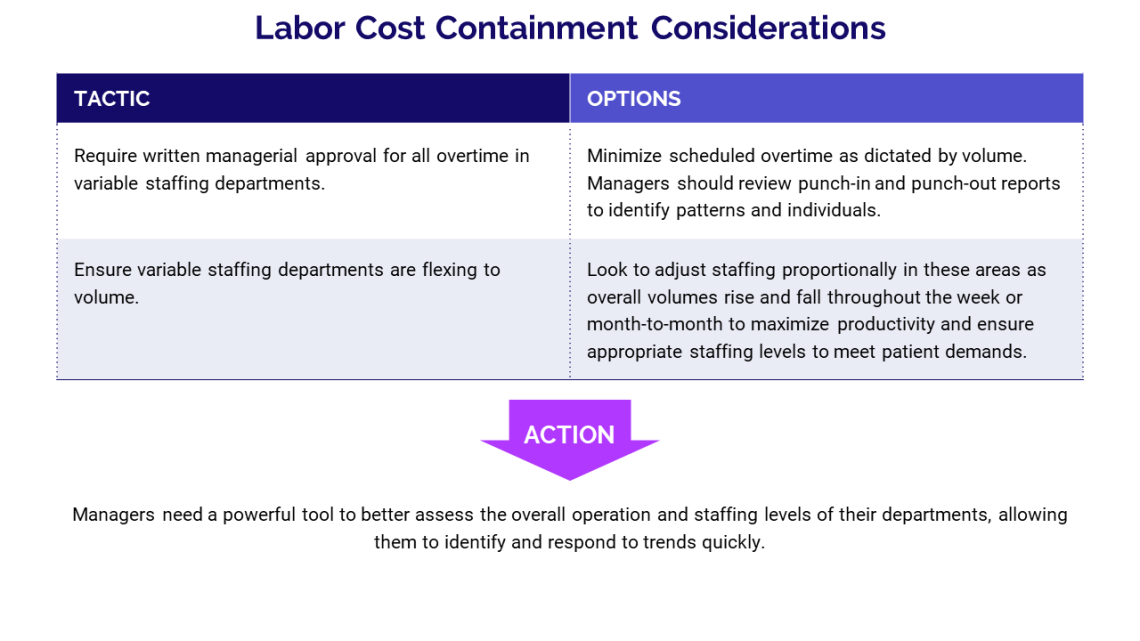
Strategy 2: Link labor costs and productivity
Labor expenses are the No. 1 driver of total costs for most departments, and increased competition for qualified healthcare professionals amid workforce shortages is pushing labor expenses higher. By focusing on productivity, managers can better assign labor resources where they are most needed to improve workflows while minimizing downtime.
By back-testing forecasting assumptions, leaders can improve the accuracy of their projections over time. Leaders also can use productivity analyses to replace assumptions from previous projections with actual driver values, which enables them to test the quality of their predictive models. They then can analyze where values differ from estimates, and how inputs may have resulted in different outputs than modeled. This analysis helps assess how changes in volumes or services affect different plan elements.
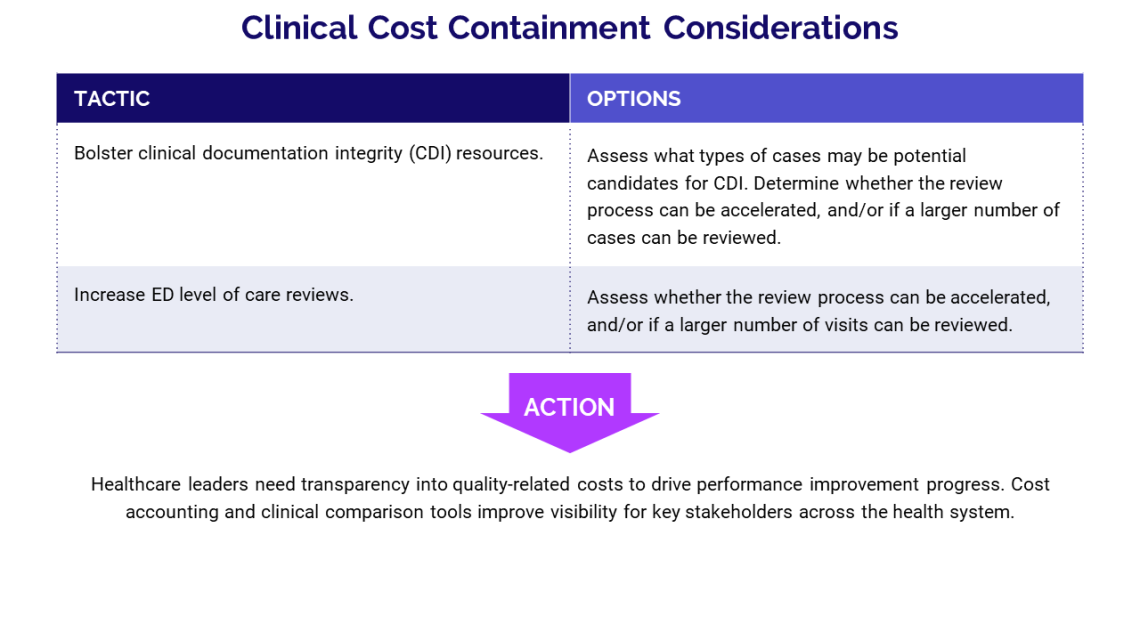
Strategy 3: Communicate the budget impact of costs associated with quality performance
Poor quality care can negatively affect patient revenues or operating expenses, but many organizations do not clearly define or account for such costs in external or internal financial statements. By including these costs as line items, leaders can track the cost effectiveness of a quality initiative and make adjustments as necessary to improve overall results. An internal cost accounting system or data and analytics platform gives healthcare leaders the tools needed to efficiently collect, analyze, and track costs tied to specific quality indicators.
By benchmarking organizational performance on quality measures, leaders can identify improvement opportunities and enhance the chances of achieving performance goals. Effective cost accounting in healthcare requires the ability to combine data related to patient care costs and quality with internal and external benchmarks.
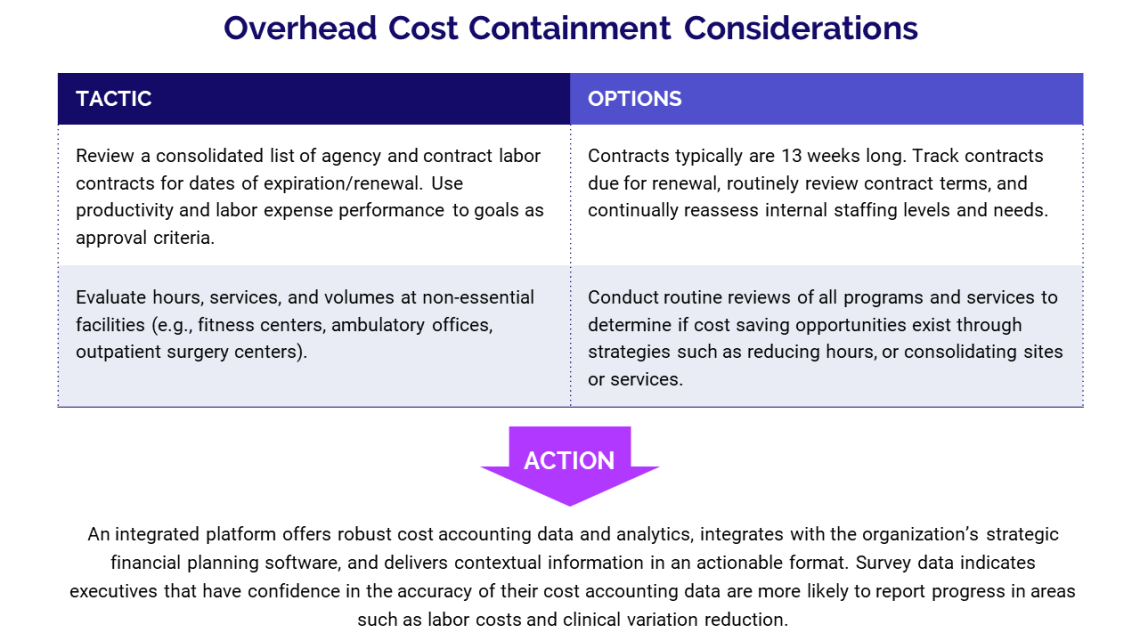
Strategy 4: Use an integrated data-driven approach to set and sustain realistic targets
To manage costs and reduce an organization’s cost structure, executives need robust, accurate data that provide insight into current hospital costs and inform decisions on how to reduce costs going forward.
Succeeding in a challenging financial environment requires a disciplined, data-oriented approach that reflects previous performance, blends financial and clinical analytics, and provides a clear understanding of how far the organization must go to ensure a sustainable path forward.
Having more data on its own, however, will not lead to performance improvements. Organizations need actionable data. Advanced analytics systems can display role-based dashboards that eliminate the need to sort through rows and rows of data. Problem areas are prioritized and displayed in context with your budget, trends, and peers in a single source of truth across multiple levels of your organization.
In years past, many hospital boards started their financial planning with the assumption that volumes would increase year over year, which meant they often could avoid tough decisions about where to cut costs. Recently, those assumptions have proven unreliable.
As hospital leaders confront the prospect of long-term expense challenges, they must establish and communicate financial targets for cost management and cost reduction initiatives to create a pathway to financial sustainability.
The imperative for hospitals to embark on continuous, organizationwide cost reduction initiatives has never been greater. With the right infrastructure and systems in place, organizations can integrate their clinical and financial management and transform their organizational approach to managing costs. Ultimately, cost reduction should be part of an organization’s DNA — a continuous journey, not a destination.
*Adapted from COVID-19 Monitoring and Planning Guide: Cost Containment, copyright 2020 Kaufman, Hall & Associates, LLC — a Syntellis strategic partner.
Learn more about enterprise decision support with Axiom
4 Essential Strategies for Cost Containment in Healthcare

How to Maximize Impact with Axiom Enterprise Decision Support