As COVID-19 continues to spread and healthcare workers heroically deliver quality care, expenses continue to climb and revenues have not yet recovered from 2020 lows, according to the 2021 Healthcare Financial Technology Trends report.
Part 1 of this series shared report highlights and how to build agility for the road ahead. This article will review how to equip healthcare organizations to address the three top challenges leaders identified in the report:
- Increasing care costs
- Mounting pressures to improve profitability
- Declining volumes across emergency departments, surgeries, and other areas
Quantifying challenges
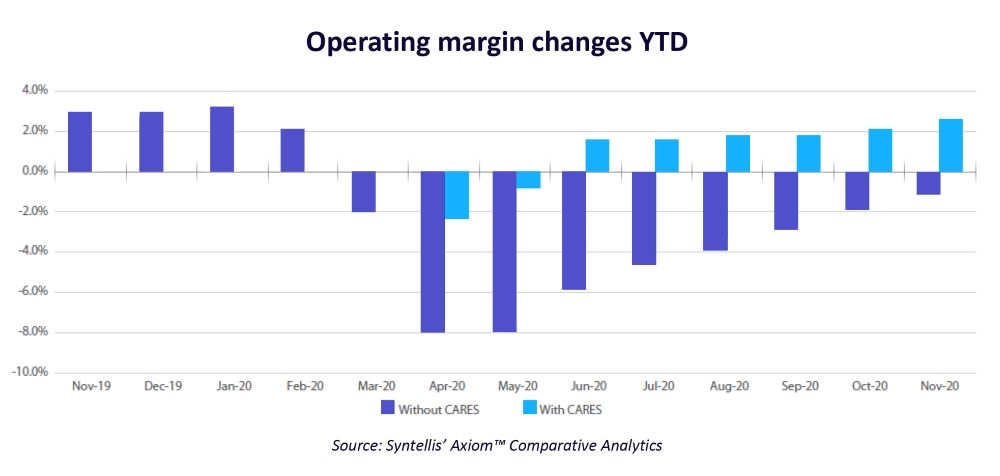
The median hospital Operating Margin dropped precipitously in the early months of the pandemic, hitting a low of -8% in April and May. Operating Margins remained below 2019 levels for much of the year, not including federal funding from the Coronavirus Aid, Relief, and Economic Security (CARES) Act (see Figure 1).
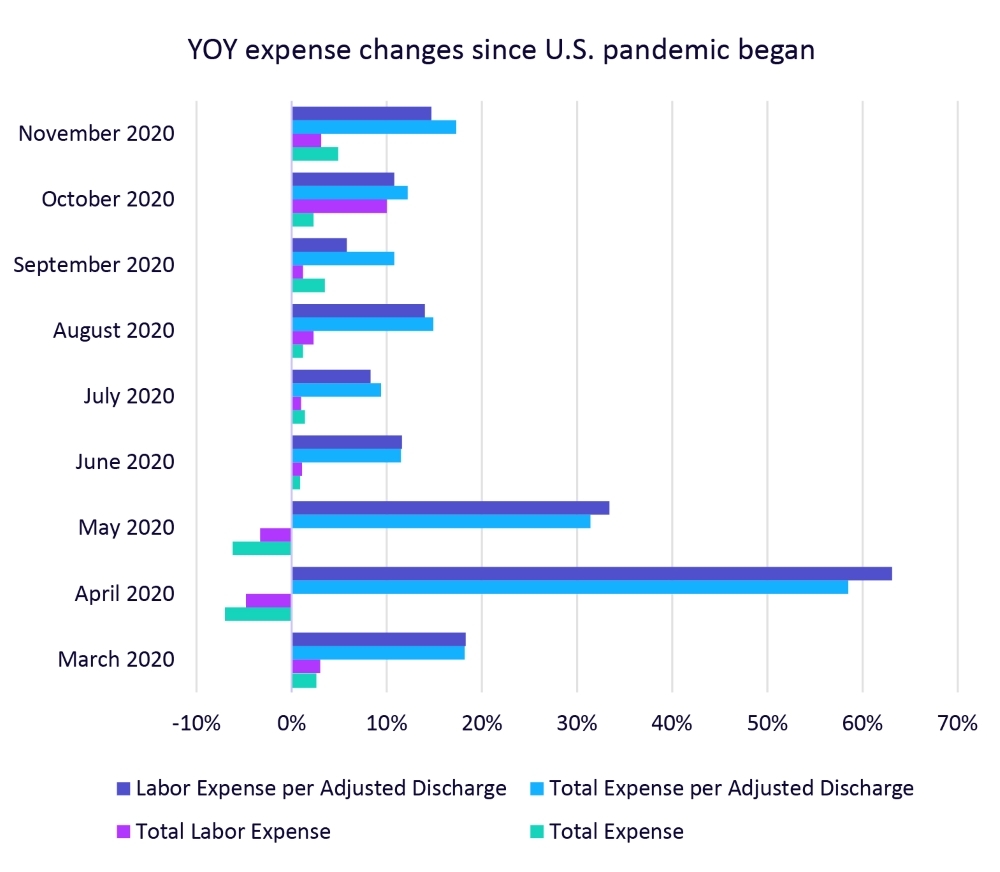
Since March 2020, Total Expense per Adjusted Discharge and Labor Expense per Adjusted Discharge remained higher than in 2019 (see Figure 2).
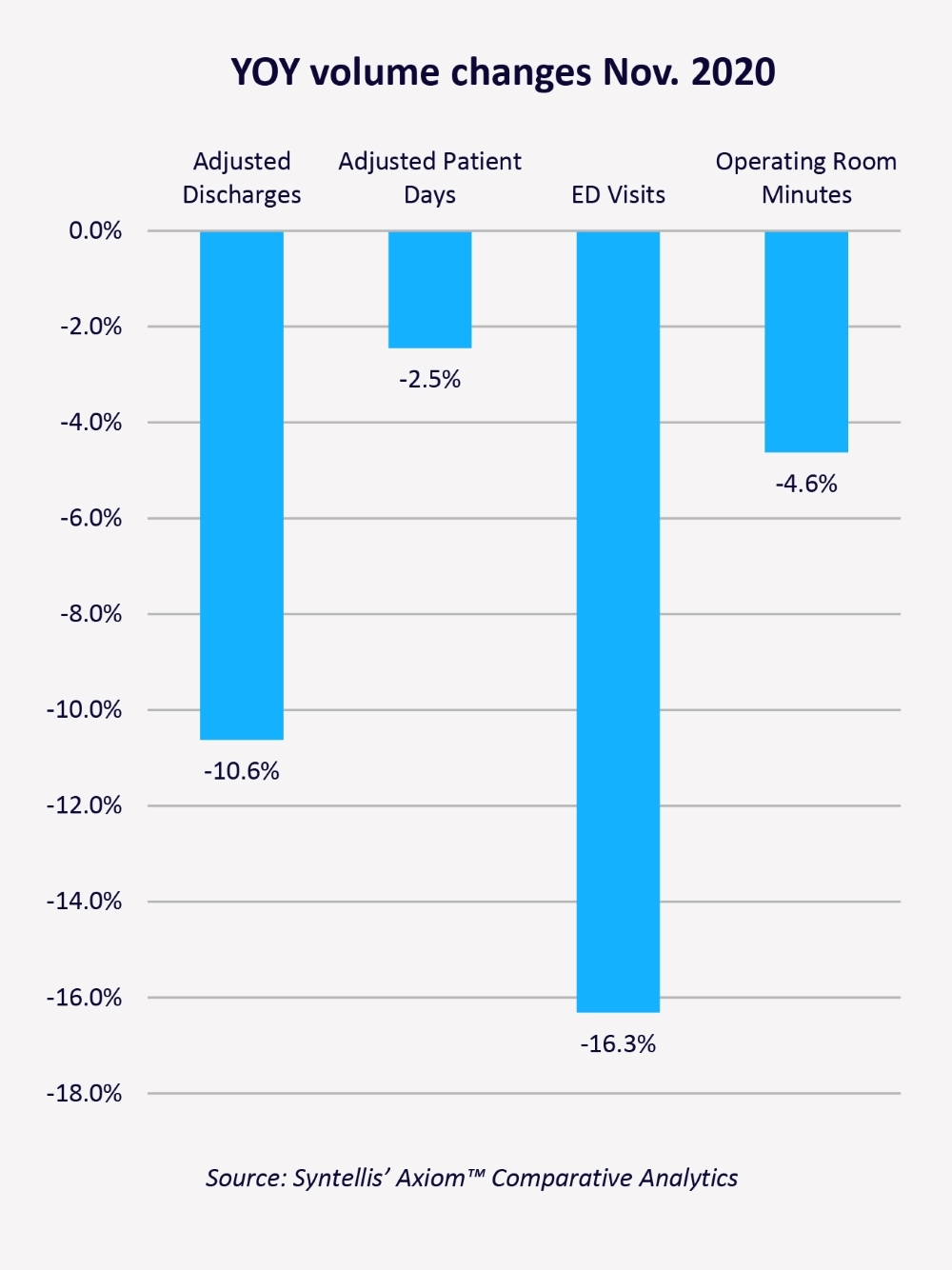
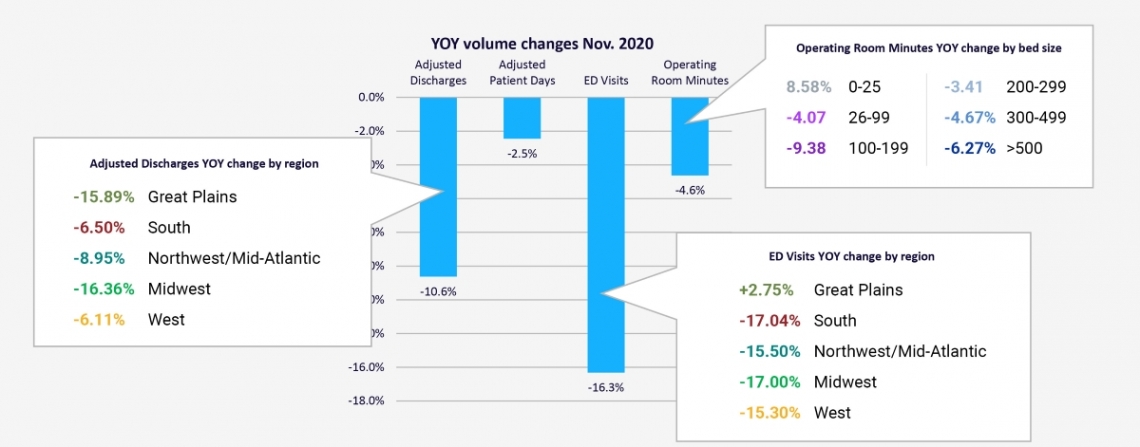
Hospitals across the country continued to see significant volume decreases in November 2020, according to the report. Emergency Department Visits were down 16.3% compared to November 2019, Adjusted Discharges fell 10.6%, and Operating Room Minutes fell 4.6% year-over-year (Figure 3).
Improving performance with the help of CARES aid and expanding access to vaccinations offer some hope for recovery, but organizations need not passively wait for things to improve. Healthcare finance leaders can take action today to help improve financial and operational performance.
Figure 1. Operating Margin Index YTD by Month
Figure 2. Year-Over-Year Expense Changes Since U.S. Pandemic Began
Figure 3. Year-Over-Year Volume Changes Nov. 2020
Effective Cost Management In the COVID-19 Era
Eighty-two percent of respondents cited cost management and reductions as very important to recovery efforts. Unfortunately, many hospital and health system finance leaders simply do not have the tools they need to best support cost management efforts — just 48% said cost accounting processes at their organizations are optimized for efficiency, accuracy, and savings.
Accurately capturing, assessing, and modeling the costs related to ongoing COVID-19 impacts is key to cost reduction in the COVID-19 era and beyond. This requires advanced costing methods that are both methodical and forward-thinking. Consider the following approach to a long-term costing configuration:
- Take an inventory of the changes made in source systems, so these modifications can be addressed within the structure of the cost model.
- Identify areas where new cost categories may be required. Common examples include PPE tracking or other revenue offsets.
- Review the clinical criteria to identify COVID-19 cases to enable the alignment of specific cost-of-care expense to the cases, where appropriate. This alignment may include targeting COVID-19 cases with the increased costs or deciding to allow a broader group of cases to absorb the cost based on the organizational view on how to reflect the increased cost.
- Consider the best source of reporting for COVID-19 tracking and whether reporting will be sourced from general ledger, clinical source systems, and/or service line analysis.
- Review the clinical coding and service line mappings to understand how these cases will be captured in service line reporting. Consider the impact of breaking out COVID-19 cases from the traditional service lines.
Using Data and Analytics to Guide Decisions
Reliable and timely data and analytics empower healthcare leaders to closely monitor performance, respond quickly to needed volume changes, and guide strategy. Yet finance leaders struggle to do so — 76% said their organizations could and should do more to leverage financial and operational data to inform strategic decisions.
Because recovery planning is a data-driven exercise, reliable and trustworthy decision support tools are critical. Decision support tools identify and compare population trends across a variety of volume, financial, and clinical measures, helping healthcare organizations easily:
- Bring together encounter-specific data (billing and clinical coding) from across the continuum of care and normalize the data to support effective analysis
- Integrate with advanced cost accounting capabilities and comprehensive net revenue modeling to establish a clear picture of financial outcomes, combined with tools to classify and analyze patients across service lines, cohorts, and illness severity
- Provide the ability to structure analyses to support line-of-business reporting and enable the effective ad hoc assessment of various user-defined populations
- Extend traditional volume and financial measures to include comparative clinical quality, safety, and patient experience measures to support ongoing engagement with clinical leaders to reduce unwarranted clinical variation and improve patient outcomes
Digging Deeper to Find Improvement Opportunities
Understanding how a local market or similar sized organizations perform and comparing those metrics to your performance equip organizations for a long and successful future.
For example, by comparing an organization’s performance to the deeper data shown in Figure 4, healthcare finance leaders can ask questions to find root causes and address them to improve performance. Key questions might include:
- How do our adjusted discharges compare to others in our region? Have we adjusted goals and plans to reflect market realities? Which service lines are contributing most to discharges?
- Are our ED staffing levels appropriate for our geographic area? If ED visits are increasing in our area, are we adequately prepared? What might increased activity in the ER mean? Is it good or bad for our organization? Might patients be waiting too long to see their primary care physician, opting for the ER instead? Do patients have sufficient access to non-acute care?
- Can we adjust OR plans to better accommodate market demands for smaller facilities? What strategies can help us reduce losses at larger facilities and maximize throughput at smaller ones?
Figure 4. Year-Over-Year Volume Changes Nov. 2020 with Detail
Many factors will influence how quickly hospitals and health systems recover from the economic turmoil of 2020 and the ongoing COVID-19 crisis. Healthcare finance leaders need the ability to identify and analyze those factors and develop data-driven solutions. This requires that organizations move away from inefficient tools and processes and ensure they have a comprehensive suite of enterprise planning management tools to optimize performance data and analytics for successful recovery.
Read Costing and Reporting Tactics for COVID-19 Recovery to learn more.
Your peers also read...
Building Agility for the Unknowns Ahead
2021 Healthcare Financial Trends Report