Across the healthcare industry, the early months of 2022 brought widespread staffing shortages, inflation, and relentless cyber threats — all compounded by the pressures of the ongoing pandemic. Together, these challenges continue to drive unexpected costs for healthcare executives.
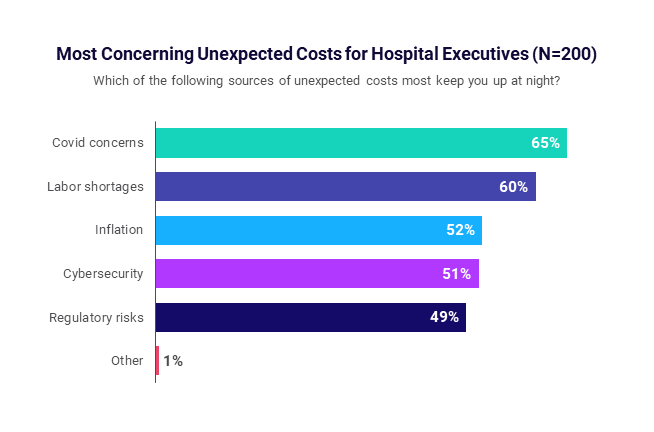
Asked which sources of unexpected operational costs keep them up at night, three in five healthcare executives cite labor shortages, while more than half (52%) point to inflation. Another 51% indicated cybersecurity, and nearly half (49%) cited regulatory risks, according to a recent Syntellis report, produced in partnership with Wakefield Research.
COVID-19 remains a top concern for 65% of the 200 U.S. hospital and health system c-suite executives surveyed. The results reflect the immense and unparalleled challenges of the current healthcare environment, and the mounting importance of cost containment strategies to ensure not just financial sustainability, but organizational survival.
Three-quarters of healthcare executives said cost containment is a high priority, yet respondents are divided on how best to manage costs. Below, we share four tips that can help healthcare leaders implement effective cost containment strategies at their organizations.
Casting a Wide Net
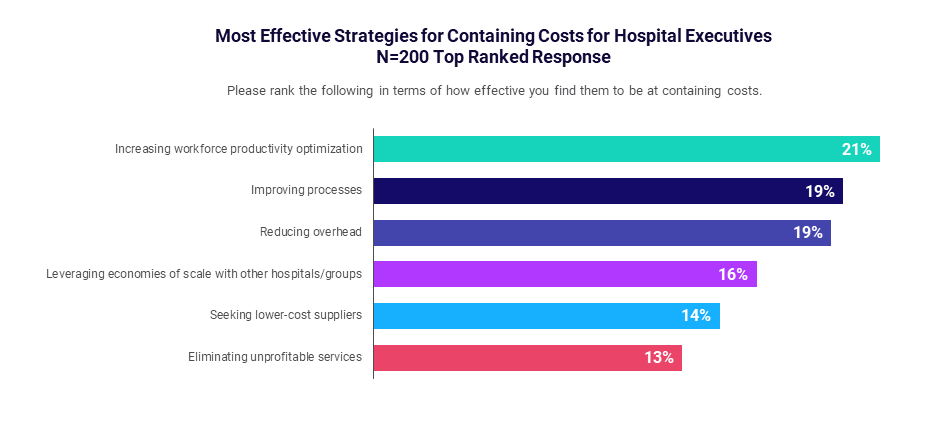
Asked to rank the most effective means of containing costs, leaders’ responses were spread across multiple key priorities. No single strategy rose to the top as a primary solution.
Optimizing workforce productivity, improving processes, and reducing overhead expenses each received about 20% of survey responses. Executives also identified leveraging economies of scale, seeking lower-cost suppliers, and eliminating unprofitable services as effective strategies.
The variety of responses shows that executives are casting a wide net to address an array of unexpected costs affecting their organizations. This approach illustrates the challenges of cost containment — creating a comprehensive strategy to reduce existing costs and control both current and future costs.
4 Tips to Reduce Operational Costs in Healthcare
How can hospitals reduce operating costs? Effective cost containment moves beyond traditional, one-off cost-cutting initiatives. While such initiatives often lead to short-term savings, the benefits wane over time or are offset by rising expenses in other areas. Instead, executives should aim to integrate cost containment as an ongoing part of routine processes.
Four tips to implement an effective cost containment strategy are:
1. Improve understanding of organizational costs. To address rising costs, healthcare leaders must first understand the cost drivers by continuously evaluating costs at all levels across an organization, including supplies, labor, facility needs, maintenance, and clinical performance.
For example, leaders should track supply chain cost and utilization data on purchased products and services through to individual patient encounters. Analysis of this data can help leaders gauge the hospital’s performance against internal and external benchmarks, project future demand, and guide purchasing plans.
2. Build engagement organization-wide. Healthcare leaders need to build a culture of cost containment that permeates the entire organization and supports ongoing performance improvement. Maintaining buy-in and input from stakeholders across different departments, facilities, and service lines helps leaders better understand cost drivers and identify realistic, sustainable targets.
Having the support of physicians and other frontline clinical and support staff is essential in developing and implementing actionable cost containment strategies, as they are the ones typically responsible for the execution of those strategies day-to-day.
3. Link labor costs and productivity. In today’s environment, labor costs can account for as much as 60% of an organization’s total costs — a critical concern amid current labor shortages.
Tying labor costs to physician and staff productivity can help uncover inefficiencies. It also helps leaders determine how best to allocate labor resources to improve workflows, minimize downtime, and ensure appropriate staffing levels to meet patient demands.
Executives should collaborate with clinical and departmental leaders to evaluate labor costs and establish reasonable productivity targets that maintain high standards for care quality.
4. Provide robust tools for data-driven decision-making. Clinical leaders, departmental managers, and others across an organization working to implement healthcare cost containment strategies need access to accurate cost data and analytics.
Analyzing and monitoring expenses, cost and utilization trends, patient volumes, productivity, and other performance metrics relative to targets require modern cost accounting, comparative analytics, and clinical comparison solutions.
The need for hospitals and health systems to implement continuous, systemwide cost containment strategies has never been greater. Ultimately, patients pay the price for uncontrolled healthcare costs. According to the survey, more than four in five executives (81%) said costs from poor planning typically are passed on to patients.
Syntellis’ Axiom Enterprise Decision Support alerts healthcare leaders to unfavorable trends, providing a comprehensive and detailed view across cost, quality, and service line measures. This granular detail helps inform decision-making to drive improved financial, clinical, and operational performance.
Your peers also read...
What’s in Store for Healthcare Organizations in 2022

Decision Support Systems in Healthcare Bring Data Visibility and Transparency