Many organizations have an opportunity to address a difficult-but-essential element of cost transformation: reducing inappropriate clinical variation.
Hospital and health system executives recognize the imperative to transform their organization’s costs as they transition to value-based payment models, strive to remain competitive, and seek to generate capital to fund strategic growth initiatives. Many organizations have an opportunity to address a difficult-but-essential element of cost transformation: reducing inappropriate clinical variation.
Recognizing an Untapped Opportunity
In a recent report on the state of cost transformation in U.S. hospitals and health systems, 86 percent of respondents said cost transformation is a “significant” to “very significant” need for their organization today. At the same time, they said the following:
- 62 percent did not cite reduction in inappropriate clinical variation as a focus.
- 46 percent cited no progress with reducing inappropriate clinical variation.
- Only 42 percent regularly delivered reports on quality, cost, and patient experience to physicians
Physicians strive to provide the best care for their patients. With solid data and insights, they can see what the best should be and where gaps exist between current outcomes and the outcomes expected of top performers.
Within these gaps lies a significant untapped opportunity for cost savings as well as gains in quality, patient safety, and patient satisfaction.
Understanding the Elements of Physician-Performance Reporting
To achieve reductions in inappropriate clinical variation, an organization must be able to provide comprehensive reporting on inpatient and outpatient outcomes, then accurately attribute encounters to the physician who is driving the outcomes.
Comprehensive reporting. Physicians must have a view across a history of encounters to understand where they consistently vary against expected performance and where they have opportunities for improvement.
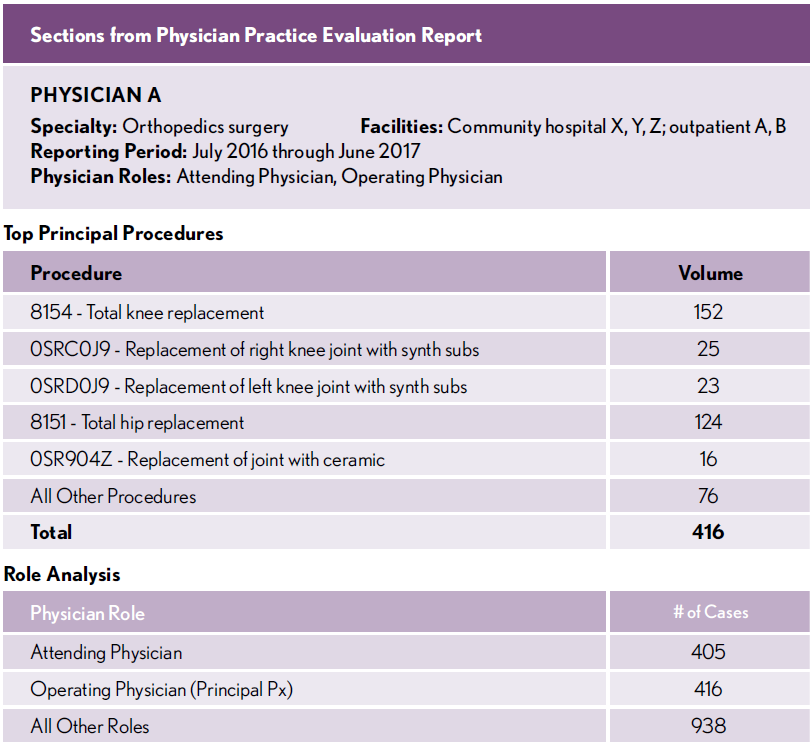
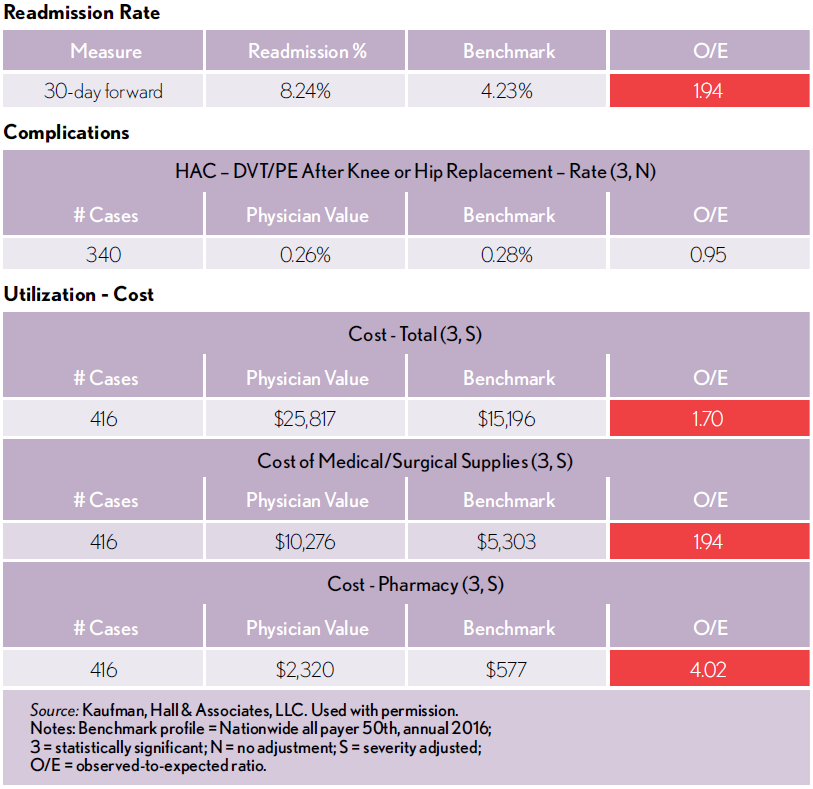
The exhibit below shows sections of a report for an orthopedic surgeon on all procedures in which the physician had a role over the course of a calendar year. Key elements of this report include:
- Analytics on specialty-specific measures as well as key analytics such as re- admission rates and resource utilization and costs
- Benchmarking to show how the individual physician varies in relation to internal and external norms
- Visualization of data that allows physicians to easily identify where their observed outcomes fall below expected outcomes
In this case, the report clearly identifies opportunities for reductions in re-admissions and significant cost savings in the areas of medical/surgical supplies and pharmacy, as indicated by the red boxes.
Accurate physician attribution. The physician of record may not be the primary driver of clinical outcomes for a given encounter. To accurately identify opportunities for improvement, an organization must also be able to identify the provider who is best situated to realize those opportunities.
This requires an algorithm that can attribute physician practice based upon encounter-level data elements including cost, orders, ordering physician, diagnostic and procedural coding, and DRGs. This enables further detailing of provider specialty practices and interactions that affect the episode of care.
Closing the Opportunity Gap
Armed with meaningful analytics, appropriate benchmarks, clearly visualized outcomes, and accurate physician attribution, organizations are well on the way to engaging their physician enterprise in efforts to reduce inappropriate clinical variation. With a data-driven understanding of how and where they can improve, physicians will be eager to close the gap where current outcomes lag behind expected performance.