Hospital and health system leaders in every corner of the United States are confronting the unprecedented, minute-by-minute challenges of the COVID-19 pandemic, from securing supplies and managing ICU capacity to keeping staff safe from exposure and rested for the next shift. While these priorities are currently consuming the lion’s share of many leaders’ time and attention, the combination of a dramatic rise in medical cases and a widespread halt of elective and scheduled procedures is simultaneously creating significant financial strain.
In the coming days and weeks, many national forecasting models currently anticipate that COVID-19 cases will gradually peak across the United States. Even while grappling with the real-time challenges of the surge, hospital and health system leaders need to begin addressing how and when to bring back currently idled services and gradually pivot to the “new normal” of the post-surge environment.
Organizations are faced with the difficult but necessary prospect of initiating these deliberations while widespread uncertainty remains about the arc of the COVID-19 pandemic. However, through careful scenario planning, organizations can begin to forecast how the pandemic’s impact might continue well after the surge, from the prospect of a relatively quick recovery to the gloomier outcome of an annual winter surge in COVID-19 cases for the foreseeable future.
Understanding potential scenarios and monitoring progress across multiple factors will help hospitals and health systems make initial decisions about reviving shuttered service lines. This approach will also help leaders begin the conversation about the long-term strategic planning needed to secure their organization’s future in a post-pandemic environment.
4 COVID-19 Scenarios for Hospitals
While many scheduled surgeries will continue to be delayed in the near term, hospitals and health systems must begin developing plans for resuming specific scheduled procedures, including determining which procedures are a priority to restart, when to resume scheduled surgeries, and where the safest places are for patients and staff to operate.
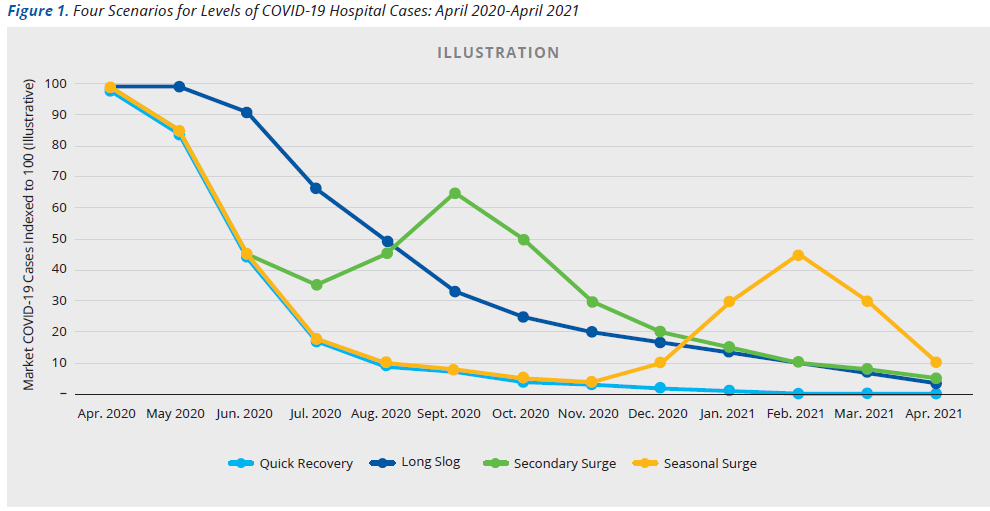
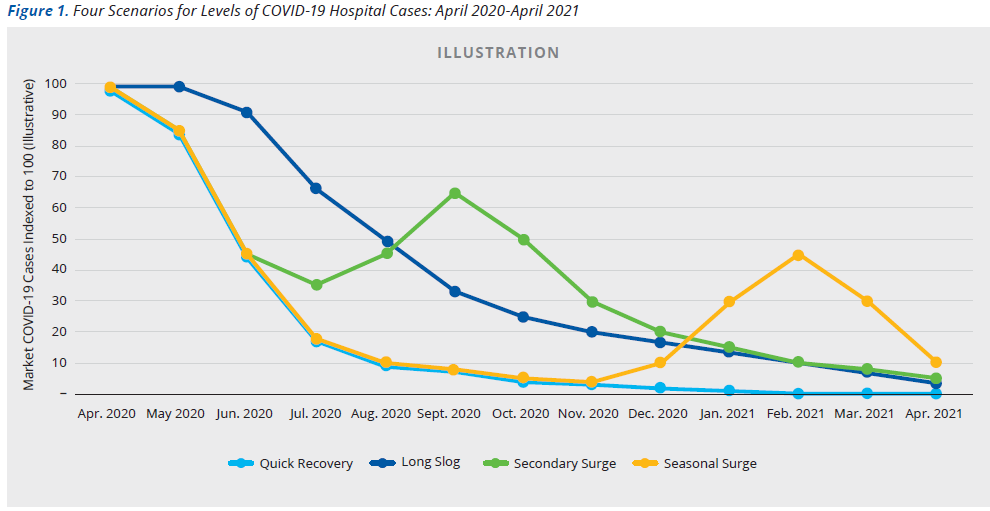
Broadly, four scenarios showing the potential impact of COVID-19 on clinical volumes can help organizations illustrate demand over the next 12 months. Though each market is unique, and the progression of the COVID-19 curve will vary greatly, the scenarios can outline unique volume implications for hospitals over the next 12 months, based on the varying timing of the surge in specific locations.
Scenario 1:
Optimistic: A quick recovery. This scenario assumes that COVID-19 cases will peak by mid to late April, will decline moderately into May, will decline sharply through the summer, and through the winter, fall, and spring will fall to near zero.
Scenario 2:
Pessimistic: A long slog. This scenario has the surge of COVID-19 cases extending through May, then declining slowing through the summer, fall, and winter, with a small number of cases persisting next spring.
Scenario 3:
Second Wave: secondary surges. Under this scenario, we would experience a peak in mid to late April and another, smaller peak in the fall, followed by a relatively steady decline in cases through next Spring.
Scenario 4:
New Normal: Seasonal surges. The final scenario assumes a relatively sharp decline in cases after April, but another peak next winter and fall, at roughly the time of the original outbreak—the expectation being that COVID-19 would continue to appear seasonally.
Figure 1 illustrates the levels of potential. COVID-19 hospitalizations over the coming year according to the four scenarios. As more data becomes available post-peak, organizations can and should update their scenarios to focus on those that seem to best fit their market’s curve.
Model Demand Based on the 4 Scenarios
In the near term, health system decision-making will continue to be driven by the immediate need to treat COVID-19 patients in facilities and locations that minimize infection and risk to exposure for other patients and clinical staff. Over a longer timeframe, organizations can slowly pivot their decision-making to address more longstanding service distribution issues. For example, facility decisions made during or after the surge to address safety concerns might ultimately serve as a catalyst for rethinking where surgery cases are managed in the future. Taking into consideration the need to maintain vigilance about safety issues, the different clinical needs of different types of procedures, and consumers’ post-COVID preferences, hospitals will need to assess the appropriate use of surgical facilities, including those on the hospital campus and freestanding ambulatory surgery centers.
The timing of this pivot will require organizations to carefully articulate and gauge the nature of the post-surge environment. A methodology that tracks the interaction of COVID-19 and non COVID-19 cases in the acute care setting can help explore progress for the four scenarios, prioritizing 5 inpatient categories:
- COVID-19 census
- The non-elective surgical census
- The medical census
- The elective priority surgical census
- The elective non-priority surgical census
Each descending priority should await consideration for resumption until a significant portion of the demand in the previous category has been accommodated. Effective methodologies will also incorporate mandated facility or state suspensions of elective procedures.
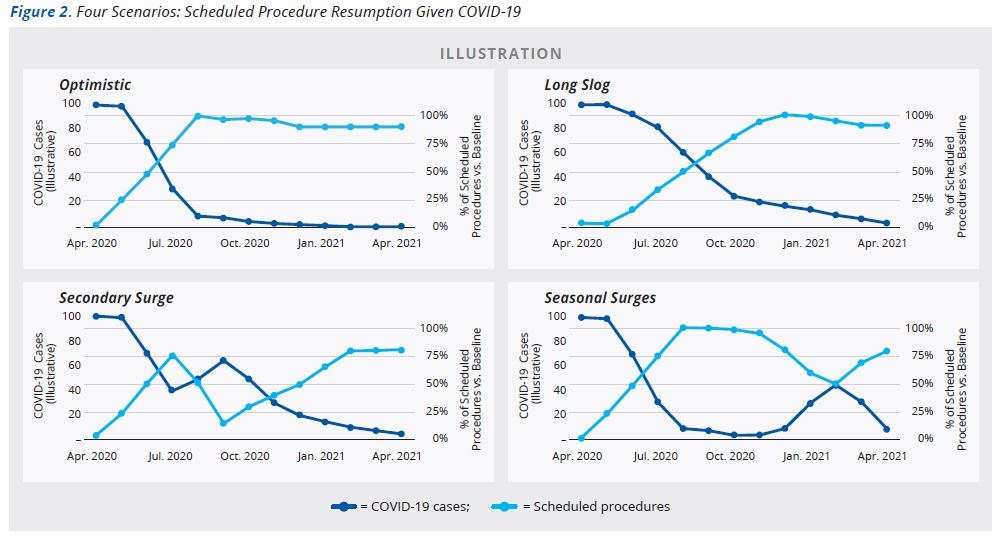
Figure 2 illustrates timing for the return of scheduled procedures under each of the four scenarios. The dark blue line (left y-axis) demonstrates COVID-19 volume, indexed to 100. The light blue line (right y-axis) illustrates the percent of scheduled procedures performed versus expected 2020 volumes if COVID had not occurred. Scenarios are illustrative and will be specific to an individual hospital and market.
Using scenario planning, organizations can start to identify the impact of capacity shortages on the elective surgery volumes that they can accommodate, including the possibility that patients will seek out services at competing organizations. While in the near-term, the widespread lack of acute care capacity may reduce the risk of losing these cases, in the mid-term, clinical necessity and financial pressure will likely cause hospitals to reopen their operating rooms if appropriate safety measures are taken.
That said, several factors will continue to exert near-term downward pressure on scheduled procedure volumes, including:
- Sustained reductions in ICU utilization to ensure the surge has subsided locally
- Rebuilding of strained supply chains
- Ensuring the hospital workforce is rested and recovered from the surge, while being mindful of the lasting trauma many clinicians may experience, especially in hard-hit areas
- Creating policies focused on containing future risks to exposure from COVID-19 in specific facilities and specific processes (e.g., separate areas of facilities for COVID-19 patients or designated surgery centers or other off-campus sites for care)
Global Considerations
Beyond the four walls of the hospital, health systems will need to monitor the volumes of new COVID-19 cases regionally and nationally, as well as the development of public health capacity to conduct widespread testing, track potential resurgences, and effectively treat and quarantine patients in multiple locations.
From a global perspective, potential signs of an improving long-term outlook include:
- Widespread, accessible, fast and accurate testing
- The development of a national surveillance system that can track spikes and falls in COVID-19 activity
- Capacity to test individuals and develop regional and community measures of exposure and immunity
- The ability to isolate, trace and quarantine patients rapidly and treat new cases at home or in the hospital
- A sustained reduction in community infections (measured by actual infections and not the rate of infection)
- The easing of local and state restrictions on travel
Imperatives for Hospital Leadership
Over the next 12 months, the uncertainty and turmoil that hospitals and health systems are currently experiencing will gradually give way to a clearer understanding of the post-surge operating environment. Guided by scenario planning and close monitoring of key internal and external markers, leaders can gradually pivot their thinking to more long-term strategic planning, as elective services resume and the proportion of COVID-19 cases begins to assume a steadier and potentially more predictable path.
These deliberations will begin to explore the delivery model and capacity requirements needed to sustain operations in the future, while effectively preparing institutions for new outbreaks of COVID-19 or potential future pandemics. At this juncture, careful planning will be needed to begin to guide the organization’s financial position and projected future performance, while making necessary strategic and competitive adjustments to ensure sustainability.
The idea of preparing for a post-COVID-19 landscape may seem light years away for leaders firmly grounded in the immediate, unprecedented challenges of managing or preparing for a patient surge. But as the pandemic’s fog slowly lifts, the value of early and sustained planning for a multitude of potential COVID-19 scenarios will become increasingly apparent to organizations looking to successfully compete and remain relevant on the other side of the surge.
For more information, contact Mark Grube.