We have better tools than ever in healthcare to advance care and improve access. But legacy healthcare organizations still have not mastered a critical competency: eliminating waste.
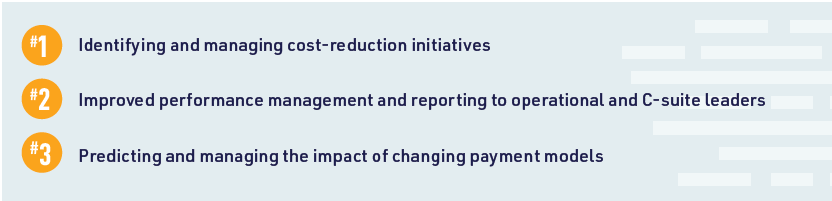
A recent study shows that 30% of healthcare spending is wasteful, at a cost of $760 billion to $935 billion.The need to reduce costs is high on healthcare leaders’ radars. A new Kaufman Hall report shows that the ability to identify and manage cost-reduction initiatives is healthcare finance executives’ top priority for 2020 (see exhibit), but they struggle to act on opportunities:
- More than half of healthcare finance executives say they don’t have the tools to lower costs in the right areas without compromising quality.
- Cost accounting systems often fail to provide the support needed to reduce costs: 43% of finance leaders say they have an existing cost accounting solution, but it’s too simplistic or they have limited trust in the accuracy of results.
Exhibit: Top Financial Performance Management Priorities in 2020
Eliminating waste is part of the solution to healthcare reform, but it cannot be the sole focus. Healthcare organizations must balance cost reduction efforts with revenue optimization and clinical quality improvement. Leaders can address all three priorities by using data to guide action that will have the most profound impact.
Dig deeper into costs by service line, department, and physician
Reining in expenses and improving margins require finance leaders to dive into drivers of waste and low profitability. Survey results show 52% of healthcare finance leaders seek to improve profitability measurement by service line, patient, and physician in 2020.
Modern cost accounting solutions that provide an accurate, comprehensive view of costs and support data-driven analysis at the activity, physician, and patient level are critical. So is access to reliable data, especially critical given that 43% of healthcare CFOs don’t trust the data their current cost accounting systems provide.
Hone your ability to uncover clinical variation
In an era of risk-based payment, healthcare organizations must have the infrastructure and tools to identify variation in clinical care processes and supplies that fuels expense and waste. Yet even as healthcare CFOs say the ability to predict and manage the impact of changing payment models is a top priority, the new Kaufman Hall report finds just 42% are seeking to improve clinical and quality analysis—capabilities that are essential under risk-based contracts.
While many organizations have tackled variation among physician preference items, changing the game on clinical performance requires robust data and analytics that not only identify clinical improvement opportunities, but also drive accountability in addressing them. For example, leading health systems are deploying clinical analytic solutions that identify the physician who made the largest contribution to a patient’s clinical outcome and create scorecards by individual physician and physician group that measure:
- Patient safety
- Quality
- Patient satisfaction
- Utilization
- Cost
Leaders can use this data to dig deeper, using severity-adjusted control charts, for example, to eliminate variation from evidence-based practices, lower cost, and improve care. These efforts not only improve quality of care and outcomes, but also increase reimbursement and incentive payments under value-based payment models.
Find creative opportunities for revenue improvement using data
Kaufman Hall survey results show revenue-increasing activities are not among finance leaders’ top three areas of focus when it comes to financial performance management, but they should be. Using data to explore new opportunities for revenue generation is key, especially when consumers are shopping for care based on quality, cost, and convenience, and tech-enabled companies are continually nipping at the heels of legacy organizations for revenue.
A Kaufman Hall survey on consumerism found:
- Nearly 80% of organizations report having no subscription-based primary care services
- One-third offer widespread online self-scheduling for existing patients, but few offer this service for new patients.
- Just 38% of respondents offer widespread “save a spot” for urgent care
- 60% offer “save a spot” for urgent care on a limited basis or not at all.
Lack of movement toward transforming patient access threatens health systems’ ability to compete against new market entrants that seem to understand consumers’ needs better than those that have been treating consumers for decades.
Healthcare leaders should look for ways to capture data around the consumer experience monthly, not just quarterly or annually. They should use a variety of sources, and compare their performance against peers by service line, treatment type, and more. This vital information will point to new investments that can not only strengthen access and convenience, but also loyalty and revenue.
Become data strong for sustainable success
Healthcare CFOs have never been under more pressure to determine high-impact ways to eliminate waste and increase revenue. Meanwhile, 95% believe their organization should be doing more to leverage data to inform strategy. In 2020, building strategic data muscle through investments in modern cost accounting, analytics, benchmarking tools, and consumer-focused data capture and analysis will be critical to legacy organizations’ success.
Originally published in HFMA’s Financial Sustainability newsletter.