A framework should clearly outline those responsible for oversight of cost transformation, as well as specific improvement teams and their objectives.
Achieving successful and sustainable cost transformation presents a complex challenge for today’s hospital and health system leaders. These efforts provide the structural underpinning of the organization’s strategic initiatives and require change across many aspects of the enterprise. Cost improvement initiatives confined to specific departments or individual services often lack relevance in today’s rapidly changing healthcare environment.
Today’s leading organizations are successfully defining strategic goals and implementing change across the enterprise to achieve those imperatives. The goal is to not only improve costs and gain efficiencies but also enact lasting operational and cultural changes that modify the way care is delivered and enhance the long-term value of services provided at an affordable price point for the communities served.
This effort requires coordination of many moving parts and collaboration among key stakeholders. Establishing a clear organizational structure for change and oversight of strategic cost improvement initiatives is essential. Without it, efforts will lack cohesiveness and fail to attain results.
Coordinating Goals
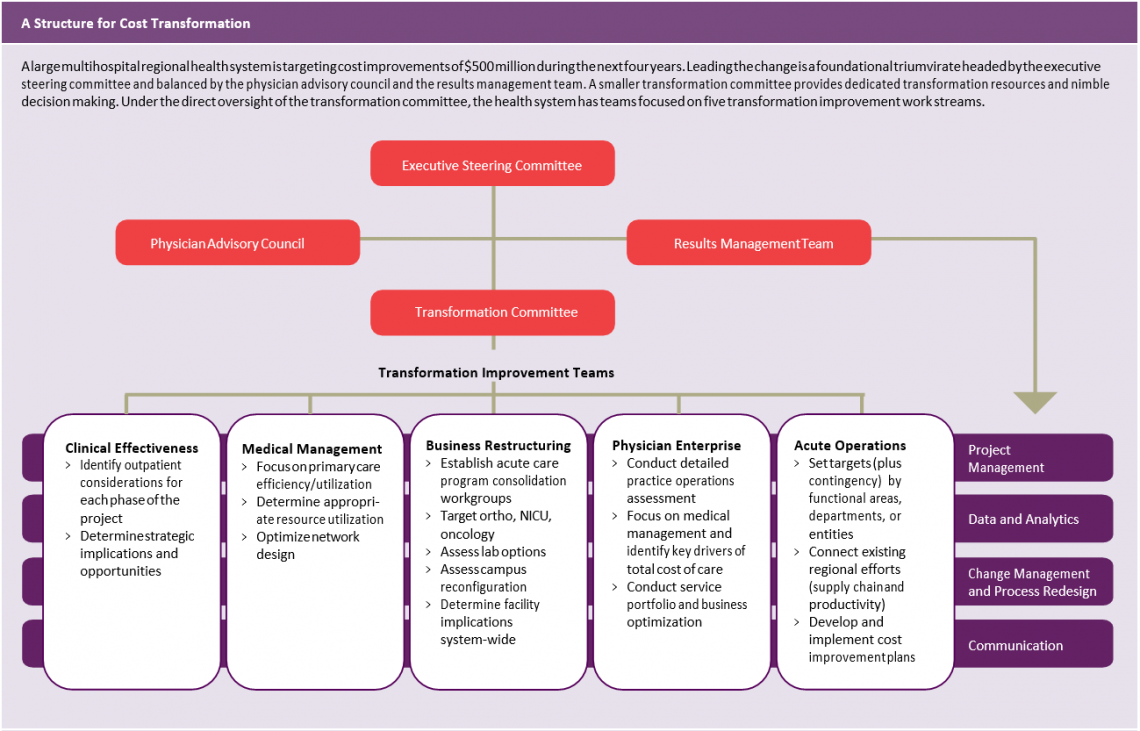
The structure for cost transformation may by individual organization and objectives. Consider a sample framework for a large multi-hospital regional health system that is targeting cost improvements of $500 million during the next four years.
Prior to undertaking the initiative, the five hospitals in the health system each had an independent operating model and structure. A large affiliated physician group established its own strategic goals that were not consistently linked to those of the hospitals, and there was no unified, enterprise-wide approach to collecting data or reporting performance results. Decisions were based largely on local considerations.
Through its transformation effort, the organization expects to align strategies across the region and decrease variation in clinical care, outcomes, and operations— and thus costs. The executive management team is committed to sharing information and best practices throughout the system.
Establishing a Structure
The example health system has a foundational triumvirate headed by the executive steering committee and balanced by the physician advisory council and the results management team. Leadership that encompasses the executive, clinical, and operational aspects of the organization bolsters buy-in from the health system’s stakeholders and ensures a high level of coordination and accountability across efforts.
The executive steering committee provides leadership and oversight of the transformational journey, seeking input from the physician advisory council and relying on the results management team for comprehensive project management. A smaller transformation committee, which also consists of a mix of clinical and operational leaders, provides dedicated transformation resources and nimble decision making. Under the direct oversight of the transformation committee, the health system has teams focused on five transformation improvement work streams: clinical effectiveness, medical management, business restructuring, physician enterprise, and acute operations.
Teams for each work stream are charged with identifying, designing, and implementing improvement initiatives that meet or exceed specific targets established to support the overall strategic goal for the system. For example, the transformation improvement team in charge of medical management is responsible for evaluating the organization’s primary care structure and identifying ways to improve care efficiencies and utilization among its primary care providers. Through this effort, the team ensures appropriate resource utilization and an optimal network design to best meet patients’ needs.
The acute operations team is focused on more traditional inpatient and outpatient services and is charged with identifying cost and operational variation across the five acute care hospitals. The team is utilizing a regional approach to identify best practices that will be used to design and implement improvement initiatives across the system. This enterprise-wide approach promotes collaboration and leverages existing expertise and resources. The team’s leadership has adopted a new motto that speaks to the transformation now underway: “Think regionally, act locally.”
Across each of these work streams, there should be sound project management, accurate and timely data and analytics, effective change management and process redesign, and clear communication with all stakeholders. The key to success is defining clear objectives and goals and reporting measurable outcomes at consistent intervals.