Data and analytics are no longer “nice-to-have” tools; rather, they underpin an organization's ability to achieve high-value care, defined as patient-centric care with improved quality and outcomes, at lower costs. Because healthcare reform—particularly Medicare reform under MACRA1—puts all providers at risk for not improving value, data and meaningful analytics are critical elements of the cost of doing business. With such tools, hospitals and health systems can drive the performance improvement needed to succeed in a value-based environment.
For most hospitals and health systems, unwarranted variation in care is a significant source of suboptimal patient outcomes and unnecessarily high costs. Such variation is present in clinical practice when there is a gap between the desired “best practice” and current practice. An analysis that excludes outliers and is risk- and severity-adjusted can indicate when quality outcomes andor costs differ significantly by physician or other care provider.This "apples-to-apples" analysis produces actionable data that can be used to eliminate or decrease the performance gap.
Causes of unwarranted or inappropriate variation may include:
- Suboptimal clinical practices or processes, such as not implementing an accelerated mobilization protocol, which is a practice expected of care providers for patients following hip or knee replacements (except in rare cases)
- Overuse of supply-sensitive care, such as higher use of specialists in regions where more specialists practice (for example, obtaining cardiology consults for all patients with chest pain)
- Misuse of preference-sensitive care, such as use of a high-cost orthopedic prosthesis or drug when a lower cost one would be equally effective or appropriate for a particular patient
- Underuse of proven effective care, such as not using prophylaxis for deep venous thrombosis with surgical patients
- Provision of services or procedures that are not clinically indicated, such as unnecessary diagnostic testing
Challenges to reducing unwarranted variation include: gaps in clinicians’ knowledge; lack of economic incentives to drive desired clinical behaviors; concerns about malpractice risk; physicians’ value of autonomy and personal preference; and inadequate decision-support tools.
A New Normal
In the traditional hospital-centric, fee-for-service environment, hospitals and physicians typically have been compensated for the care they provide, even if such care creates unwarranted variation in quality and/or cost.The value mandate from both private and public purchasers is rapidly changing this situation, putting a high-intensity spotlight on unwarranted variation in care, and providing incentives or penalties to reduce such variation.
Now becoming the norm with all healthcare purchasers, “value-based purchasing” involves performance-based payment strategies that hold providers accountable for both care cost and quality by linking financial incentives to providers' performance on a set of defined measures. Such purchasing brings information on the quality of healthcare, including patient outcomes and health status, together with data on the dollar outlays going toward healthcare. It focuses on managing the care system to reduce inappropriate care and unwarranted variation.
Hospital board, executive, and medical staff leadership must tackle this problem;it can no longer be treated as a "third rail" Use of national, regional, and organization-specific benchmark data can identify opportunities to reduce inappropriate variations in clinical practice in both inpatient and ambulatory settings.
Assuring Credible Data
An organization-wide approach to reducing clinical variation must be supported by a commitment from the leadership team to aggregate, analyze, and disseminate credible data related to quality, outcomes, and cost. Benchmark data and advanced analytics using such data enable the organization’s leadership and quality teams to compare performance against a variety of factors, including:
- Historical trend performance andor performance targets: This assessment looks at the performance of the hospital or health system using the organization’s own data overall, or by hospital, department, physician, treatment type, patient diagnosis, or other considerations
- Peer group comparisons: Data from public and commercial sources enable comparison of the organization’s performance with that of an appropriate peer group, defined as one being of similar type with like functions, services, operating revenue, or other factors. Using benchmark-based reports and scorecards, hospital executives and managers are able to observe patterns of performance based on factors such as diagnosis, co-morbidities, treatment type, department, and physician. Areas of undesirable variation can be explored and targeted for improvement.
Determining Early Areas of Focus: Case Study
One health system with three hospitals and approximately 300 affiliated and employed physicians sought an assessment of its performance compared to peer organizations on selected utilization, quality, cost, and patient safety measures. The goal of the assessment was to enable the health system to identify areas where it should focus its early clinical variation-reduction efforts.
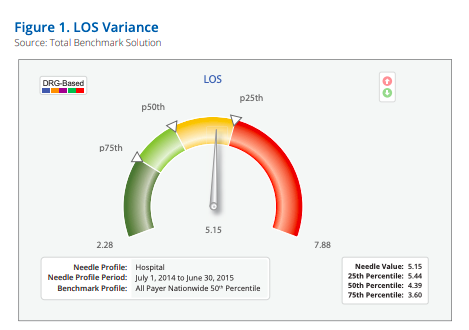
The health system used data from its own performance record, and that of public and proprietary databases.A robust analytic platform with more than 2,000 performance indicators enabled a view of how the system performed internally over time and comparatively with other organizations in the region and nation. Peer organizations were drawn from more than 5,000 hospitals nationwide. Measures included length of stay (LOS), mortality rate, critical care utilization, emergency room admissions, hospital-acquired conditions, and cost.
Based on all-payer data for the most recent 12-month period, in comparison to data from all hospitals and a regional community hospital subset nationwide, the organization was performing below the 50th percentile with LOS (Figure 1) and mortality rates, and below the 25th percentile for critical care utilization.The data were severity and risk adjusted. Analytics identified specific departments, clinical conditions, and physicians who accounted for the greatest performance variance.
Employing a data-driven approach will be critical to successfully engaging physicians in reducing care variation. Data credibility is the essential foundation for driving behavioral change. Physicians who receive reliable data with evidence of unwarranted variation in their own care—whether related to quality, outcomes, and/or cost—typically need no further inducement to bring their practices in line with their colleagues.
Where to Start
Building a sustainable program to eliminate unwarranted clinical variation can be undertaken one step at a time.The focus initially may be on an individual diagnosis-related group, or on use of a certain drug, device, test, procedure, condition, work process, clinical program, or other element of patient care prioritization of which areas to tackle first can be based on a number of factors, including likelihood of early success, magnitude of the benefit/opportunity, resources required to effect change, and expected implementation timing.
Based on such a prioritization exercise, certain datameasurement categories typically offer insights into the most significant opportunities to reduce unwarranted care variation. For example, a few of the major categories of resource utilization are as follows:
- Medical/surgical supplies: physician preference items often have high cost differentials
- Pharmacy: brand versus generic drugs and drugs for certain therapies have high cost differentials, at times without effectiveness differentials
- Accommodation: LOS can indicate physician and staff practice patterns and processes that positively or negatively impact how patients move through the hospital and discharge
- Laboratory and pathology: standing orders for daily tests, for example, may or may not be needed/appropriate
- Imaging: the physician's choice of imaging options, including MRI, CT, ultrasound, and X-ray, has a large impact on cost
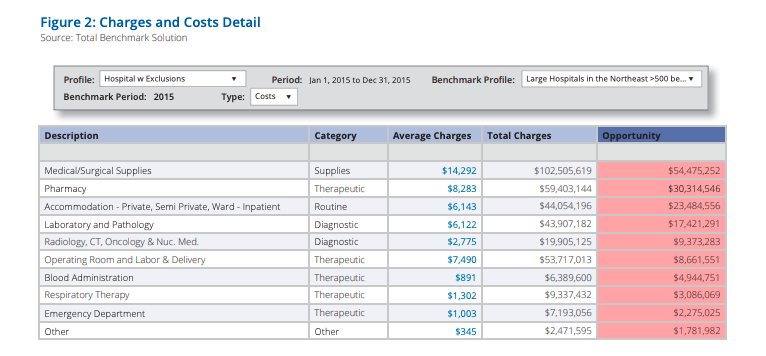
For one $3 billion hospital system, benchmark data of peer-group large hospitals in the northeast indicated the size of the improvement opportunity in these and other categories (Figure 2) For the top five categories, the hospital system had costs that were approximately $135 million higher than its peers.
Looking at its own data across the top five measure categories and total cost, the organization was able to identify which physicians had the most significant opportunities to reduce variations in care.All Patients Refined Diagnosis Related Groups (APR-DRG) data were severity adjusted, and outliers were excluded.
When compared to their peers, three physicians in different specialties accounted for nearly 2 million in potentially unwarranted care variation.This variation represented10-20 percent of the total variation and spend in each of their service lines.The opportunities to reduce variation and costs in medical/surgical supplies and imaging were particularly notable.Further assessment of spending by category indicated specific products that might be adding unnecessary cost and/or variation from patient protocol.
Physician 1, for example, used more anesthesiology supplies per minute than his peers, and the highest-cost surgical mesh. As was the case in this hospital, oftentimes physicians simply are unaware of the cost of the items, tests, or drugs they order, and can shift their ordering behavior without impact on the patient.
Drilling Down to Identify Best-Practice and Best-Improvement-Opportunity Performers
Even more powerful analytic work looks at the relationship between care quality, patient satisfaction, and cost indicators by hospital and physician. Reducing unwarranted variation in knee and hip joint replacements has been an area of focus nationally, and therefore presents an important place for organizational focus in this regard. Effective April 1, 2016, the Centers for Medicare & Medicaid Services (CMS) rolled out a new mandatory bundled payment program. Called Comprehensive Care for Joint Replacement (CJR), it involves approximately800 hospitals in 67 markets and covers nearly one-third of all hip and knee replacements for Medicare patients nationally.
The program incentivizes hospitals to optimize inpatient care, streamline postoperative care, and to discharge patients to lowercost settings or directly to home when appropriate.Hospitals are responsible for charges within 90 days of discharge.If costs are below the target rate set by CMS, hospitals keep the difference; if above, hospitals pay the difference. CMS caps losses (and gains) at a percentage of the target price. This program puts hospitals at financial risk for payments to physicians and post-discharge providers, not just for the “index hospitalization” services.
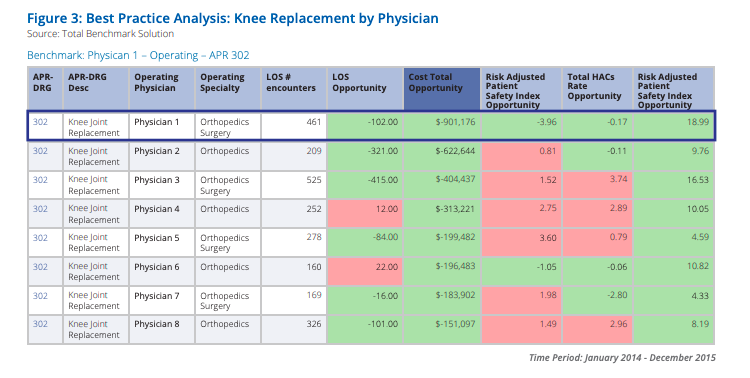
A "Best-Practice Analysis" for one multihospital system identified the best-performing hospital in the system based on indicators including length of stay; total cost; a risk-adjusted patient safety index including pressure ulcer rates, post-operative infections, and others; the hospital-acquired condition (HAC) rate; and a patient satisfaction rating. The benchmark was based on all-payer data for short-term acute care facilities nationwide.
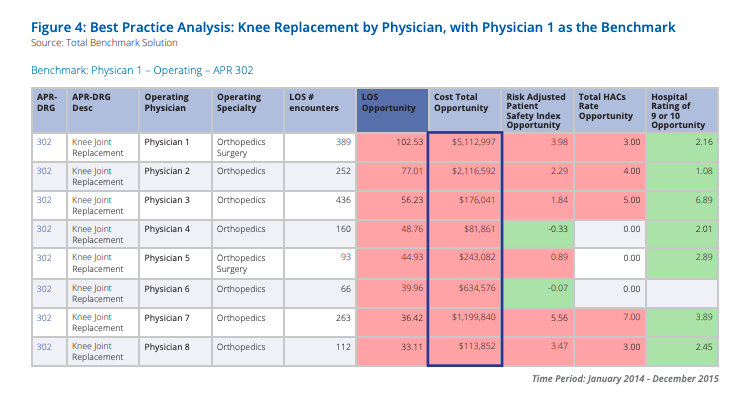
Drilling down within the best-performing hospital, the analysis identified the best-performing operating physician for knee joint replacement using the same indicators. Based on data covering a two-year period, Figure 3 shows the results for eight physicians, highlighting that Physician 1 performed above the national all-payer benchmark on all dimensions.
Next, the system requested further drill-down analytics to learn what the improvement opportunity might look like if the lowest-performing physicians performed at Physician 1’s level. Figure 4 shows those results, which would bring nearly $10 million in cost reduction opportunity.
The health system's chartered clinical improvement team closely studied Physician 1's clinical practices to learn specific means by which he was able to better assure patient safety and quality while reducing surgical and related hospital costs. Directed by physicians, with participation from nurses and other clinical team members, this is the hard work that needs to be done to reduce unwarranted clinical variation in hospitals and other facilities nationwide.The benchmark data and analytics identified the target.
Hospital leaders need access to credible and accurately attributed data and analytics that enable them to identify significant opportunities to improve financial and clinical performance, and the root causes of suboptimal performance that require corrective action. Armed with the ability to simultaneously access utilization, quality, patient satisfaction, and cost data, and benchmarks to internal and external best-practice care, executives can quickly identify underperforming areas to which attention should be directed.
To understand and improve their performance, credible and accurately attributed data and analytics are equally important to physicians and other clinicians.
The right tools are critical to the achievability of efforts to reduce unwarranted clinical variation.Is your organization accessing the best possible benchmark data and analytics to identify and make the needed improvements to quality, outcomes, and cost?
You also might be interested in...

Valley Health Charts Its Future with Axiom

Financial Planning and Decision Support Software for Healthcare Organizations