As hospitals and health systems nationwide cope with persistent workforce shortages, many are also gradually shifting leadership structures.
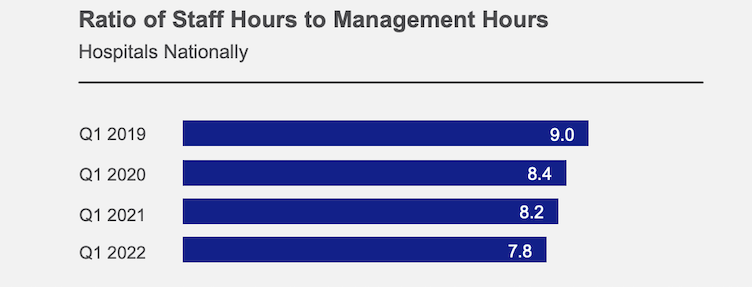
Data from more than 1,000 U.S. hospitals and health systems reveals a slow decline in the number of hours worked on non-management-related duties relative to hours worked on management dutiesi, according to a recent report from the American Hospital Association (AHA) and Syntellis Performance Solutions. The ratio decreased from nine staff hours for every one management hour (9:1) in Q1 2019 to 7.8 staff hours for every one management hour worked (7.8:1) in Q1 2022 (Figure 1).
These trends emphasize the need for robust productivity reporting and management capabilities as healthcare leaders balance efforts to control rising labor costs with patient demand to ensure continued high-quality care. Nearly three-quarters of U.S. healthcare finance leaders identified workforce optimization and workforce productivity as top priorities for building fiscal health in 2022, a national survey by Syntellis found.
Nursing Services Most Affected
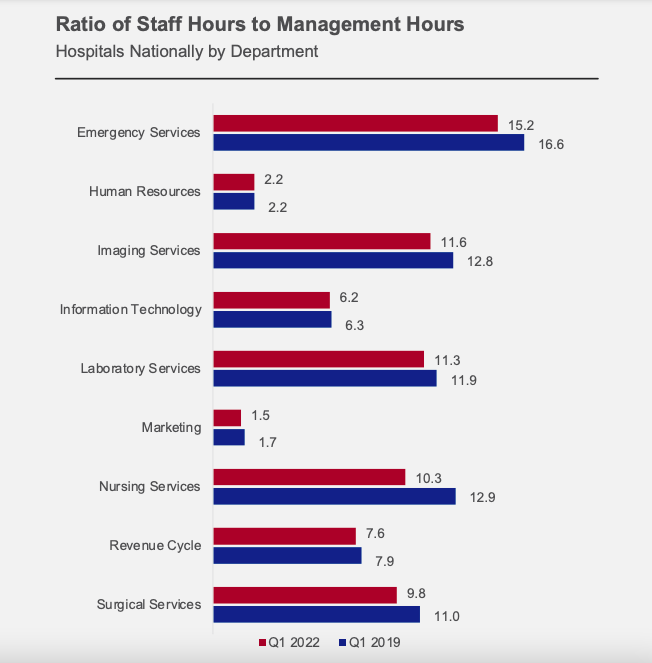
Looking across different departments, the AHA/Syntellis analysis found that Nursing Services had the most significant change over the three-year period. The ratio of staff to management hours decreased from 12.9:1 in Q1 2019 to 10.3:1 in Q1 2022. Similar declines occurred across multiple hospital departments (Figure 2). Human Resources was the exception, holding steady at 2.2 staff hours worked for every one management hour over the three-year period.
Numerous factors may be contributing to the declines, the report says. The trend could reflect managers taking on additional duties due to increased staff vacancies and the high costs of contract labor, or to help manage care due to limited visitation. Not all organizations are experiencing a reduction in management scope — the trend also could reflect retention efforts to help alleviate burdens on nurse managers and keep valuable caregivers.
Hospitals and health systems nationwide saw patient volumes grow in recent months due to pent-up demand from care delayed during COVID-19 pandemic surges. The higher volumes put increased pressure on healthcare leaders to address vacancies in nursing management. As a result, many leaders are getting creative with recruitment and retention by partnering across their organizations to reduce administrative burdens and other challenges for nurse managers and optimizing care delivery teams so clinicians work at the top of their training and education.
The overall goal is to support nurse managers so they can focus on their management responsibilities and support frontline caregivers.
Ensuring Effective Productivity Management
Managing productivity is critical to controlling rising labor costs. Nurse managers and other leaders want to staff appropriately for fluctuations in patient demand, especially given strains on staffing from ongoing labor shortages.
Productivity reporting provides managers with timely and accurate labor analytics to help guide staffing decisions. Four essential elements for effective productivity reporting and labor analytics include:
Accurate workload driver computations. Department managers should be directly involved in developing workload calculations through a centralized labor cost modeling system. Such a system enables managers to easily access and review charge item-level drivers and make updates for accuracy. The system also should store workload calculations for comparisons over time.
Fixed and variable productivity targets. Productivity targets should include assumptions for staff on both variable and fixed schedules to account for salary differentials and help tie reports back to total staffing numbers and budget assumptions. Healthcare leaders should be able to adjust targets over time to align with internal or external benchmarks.
Correlations with other analytics. Labor productivity data should be considered in conjunction with other important key performance indicators, such as care quality and patient safety indicators. Putting these analyses in a broader context helps leaders better assess the impacts of staffing decisions.
Management feedback loop. Nurse managers and other leaders need the ability to share input on labor productivity reports with stakeholders, such as explaining potential factors behind any variances and summarizing corrective action plans.
Effective productivity reporting and management can help healthcare leaders maximize limited resources amid workforce shortages and shifts in management scope. It can help organizations develop actionable staffing targets, and build buy-in from department-level managers by better equipping them to make vital decisions as they optimize their workforce and provide continued high-quality care.
Source: iStaff (non-management) contains all staff hours for employed and contract workers who are not responsible for supervising others, as well as 50% of supervisors’ hours that do not include management duties. Management hours refers to hours worked by individuals managing employed and contract workers. (Syntellis and the American Hospital Association: Quarterly Market Analysis: Q1 2022, July 2022.)
Learn more about comparative analytics
Wage Increases Drive High Hospital Labor Costs Amid Workforce Shortages