Your Complete Guide to Cost Accounting in Healthcare
101: The Basics of Cost Accounting
What is cost accounting?
Cost accounting at the most basic level assesses the cost or value of a product or service. Determining the cost of various components that comprise an end-product is useful for price setting, cost control, negotiations, and analytics. Cost accounting may involve different techniques, depending on the industry.
What is cost accounting used for?
Organizations use cost accounting data for many purposes. Understanding the underlying cost of the products and services produced allows an organization to review and assess financial performance at a granular (per unit) level and a higher level (product line, location, or other classification). Cost results can be used to assess or set prices. Knowing detailed cost results enables more successful contract negotiations — with vendors, contractors, and providers. Costing knowledge also brings informed decision-making at both the tactical and strategic levels.
What are the advantages of cost accounting?
Without cost accounting, organizations are left with two options — relying on General Ledger data or homegrown “back-of-the-envelope” analytics. Both approaches to decision-making are risky.
While General Ledger represents a true cost, the detail level is too high for informed decision-making. Department and account data often lack the nuance of quantity and cost per unit spread across many units. Rudimentary analytics using Excel can be error-prone and subject to the whims of the person performing the calculations.
Cost accounting determines an accurate cost per unit at a granular activity level, such as CDM codes for a hospital. The cost is broken out by cost categories (labor, supplies, capital, etc.), thus simplifying the costing process while enabling aggregation at meaningful levels. Costing methodologies apply basic mathematical principles and sophisticated technology to calculations to ensure accuracy, repeatability, and reliability.
Why are direct costs so important?
Direct costs drive most analytical reviews and are the costs that are within managers’ control. In healthcare, direct costs can include physician and nursing labor, medical supplies, equipment costs, and more. When calculating cost per unit, direct cost categories are where the primary computations take place. Categorizing GL costs correctly and using the most appropriate, best costing methods are fundamental steps to achieving reliable results.
Why do companies allocate indirect costs?
Many of an organization’s costs are indirect, not directly tied to the product or service but important to capture to make accurate pricing decisions. In the case of healthcare, indirect costs support direct patient care activities. Examples include accounting, collections, human resources, and IT. To fully cost patient activity, these indirect departments allocate their costs using meaningful statistics through the cost accounting process.
82% of healthcare finance leaders cited cost management and reductions as very important
to helping their organizations maintain or rebuild their fiscal health,
but less than half said their cost accounting processes are optimized for efficiency, accuracy, and savings.
201: Healthcare Cost Accounting
What is cost accounting in healthcare?
In healthcare organizations, cost accounting is used to determine the cost of each service or product used in patient care, providing detailed information that can be used for analytics and decision-making.
For example, the cost of an X-ray includes labor, supplies, depreciation, and overhead. Analyzed along with other information (e.g. charges, payments, clinical information) on a patient’s transaction record, a complete picture of a patient visit emerges. The data can be compared to payer rates to determine whether costs are in line with expected reimbursement to make pricing decisions. The same data can be parsed a different way, aggregated by provider, for example, to assess the provider’s performance against peers. Cost data is also useful in facilitating staffing decisions, informing capital request decisions, exploring new services, and more.
Healthcare costing methods
There are several methods to consider for calculating cost at your hospital or health system. This decision point is, in some ways, the more critical focus when designing a costing system or responding to a major organization initiative. When selecting a cost method, consider the type of item being costed, the resources available for the cost calculation, and the accuracy desired in the results. Cost items are typically chargemaster (CDM) codes but can also be items such as CPT codes or the pseudo cost items created through the Axiom Direct-to-Encounter utility. Traditional costing approaches include Ratio of Cost to Charge (RCC), Relative Value Unit (RVU), and Relative Cost Unit (RCU). These methods are well-known and frequently used in healthcare. These more basic methods can be used for indirect costs, areas where scrutiny of results is less of a focal point, or where resources are limited in some way. In addition, Axiom offers several advanced costing methods for areas that need a more refined approach.
Which method of cost accounting is used in hospitals?
- Ratio of Cost to Charge (RCC) spreads General Ledger (GL) costs across a set of service items in a department. While simple to maintain, RCC can lead to inaccurate results in instances where the prices do not align with resource utilization.
- Relative Value Unit (RVU) also spreads GL dollars in the department, but the basis is a value that indicates relative resource utilization. Organizations that have a reliable process for keeping RVUs up to date get more accurate cost results.
- Microcosting assigns the actual vendor cost of items when that data is available. The cost can be at the chargeable item level or at the actual transaction level.
- Markup is an alternative to microcosting where an organization can back into this cost if the markup rates are available.
- Direct to Encounter costing is a sophisticated costing method that can be used for labor costs when the resource use and the average hourly rate are known. This approach can also be used for indirect costs that directly impact patient care, thus minimizing the “overhead” bucket of costs. This targeted costing method creates a high degree of confidence in the resulting cost data.
- Activity-Based Costing (ABC) is used to ensure that cost is assigned as it is incurred through activity measures. In addition to the Direct to Encounter method noted above, costs can be assigned to specific activity measures by leveraging detailed resource data feeds such as surgical suite utilization times, resource utilization tracking, average hourly rates, and other clinical metrics. Tracking these activities and costs allows an organization to precisely assign the true cost of a service to the patient, thus creating very precise and reliable cost results.
Advanced healthcare cost allocation methods
The advanced cost calculation methods in Syntellis’ Axiom™ Cost Accounting offer options to users depending on what data is available to support the calculations. Microcosting, Reverse Markup, and Activity-Based Costing each offer advantages over the more basic methods of RCC and RVU, so it is important to consider the pros and cons. With Microcosting, the vendor cost can be assigned directly to the cost items or to the actual transaction level for encounters. This highly accurate approach increases transparency and buy-in from stakeholders. The source data from vendors is the assigned cost, which may not always be readily available. When the data is available, this approach can take your costing for supplies, implants, drugs, and even salary to new levels. Any resulting variance to the general ledger can be included or excluded from the cost process, giving users important flexibility. When possible, assigning this vendor cost at the actual encounter transaction level (transaction microcosting) is highly recommended to enable better trending and analytics. A recurring data feed with the vendor cost is required to enable this method for large groups of cost items.
Using the reverse markup method, an organization can leverage its markup policy to back into the vendor cost when the vendor cost is unavailable. This method is not as accurate as Microcosting but does offer efficiency since it requires less maintenance and no detailed data feeds.
In addition to these advanced “assignment” methods, an expansion of basic RVUs to the more strategic areas of focus can be leveraged to increase accuracy and reliability of the RVU allocation approach. This expansion should include detailed time-and-motion studies at the charge item level to ensure reliable results for labor allocations using RVUs.
Direct-to-Encounter is another advanced method that enables an activity-based approach to allocating indirect costs to the direct patient care activities. Letting activity drive cost calculations for patient-related costs that are stored in indirect departments increases accuracy and reliability for the resulting analytics. For example, Surgery Scheduling is an ideal candidate for Direct to Encounter since the cost is easily attributed to surgery cases.
When used in conjunction with “standard” costing techniques — such as RCC, RVU, and RCU — activity-based costing enables hospitals and health systems to know more precisely what a patient’s costs are. The trick is to keep this view of patient cost aligned with the organization’s overall profitability view. Activity-based costing techniques have some inherent limitations that must be well understood. Techniques that assign cost based on anything other than the general ledger can lead to variances that will need to be addressed and explained to users, particularly if the organization has always relied on GL-based cost accounting techniques. The general ledger is impacted by accruals, timing, and non-recurring entries. These items may not flow into activity-based costing calculations, leading to a gap that must be addressed.
All costing is an art form and there will always be some degree of smoothing or averaging. The goal of a good costing system is robust analytics that can lead to more reliable decision-making at the service line and other levels, plus increased precision of physician-, payer-, and procedure-level profitability data.
Timing options for cost modeling
Change and disruption are likely to be the norm for healthcare organizations going forward. Given the significant business disruption in recent years and COVID-19, as well as the resulting impacts on both volumes and costs, cost modeling may not always follow normal trends and will therefore have continuing downstream impacts on reporting. Syntellis’ Axiom™ Cost Accounting supports a variety of costing approaches and methodologies designed to more precisely attribute costs to patient care activities.
While new methodologies are being introduced to support more granular encounter-specific costs into the cost model, a significantly higher amount of direct patient care and overhead cost is being assigned to a cost item level in a cost-per-unit calculation. The goal is to ensure that the trending and ability to analyze cost is accurate and reflects the cost of providing care, regardless of the disruption going on around an organization. To this end, Axiom Cost Accounting offers several options for the timing of cost calculations. Each option has different implications for encounter reporting.
Year-to-Date Costing
Calculated cost is stored for the full year-to-date (YTD) period, recomputed with each costing run for YTD costing; per-unit costs by cost item and cost category are computed each period using YTD dollars and volumes. For example, if you run costing for nine months, the system would calculate the cost as an average over the full nine-month period and store this in the resulting cost set. These values would then be assigned to all encounters in that nine-month period at the cost item level. This approach can be processed monthly, quarterly, or annually using the cumulative proceeding months.
Reporting implications: This method provides a consistent per-unit cost across time periods, which can be used to identify cost trends or utilization variation at a cohort or across physicians. Because the per-unit cost is constant, the differences in costs within the time period can be attributed to shifts in utilization and not unit cost rates. The disadvantage to this approach is that any cost shifts occurring at an operational level are averaged and are not highlighted in any given period, thus negatively impacting true trending of cost fluctuations.
Monthly Costing
Calculated cost is stored uniquely for each month. For monthly costing, per-unit costs by cost item and cost category are computed each month based on the volumes and dollars for that specific period and stored specific to that month in a unique cost set. This enables detailed trending of the cost changes over months.
Reporting implications: If the goal of encounter reporting is to best capture how costs are shifting operationally from period to period, this method is preferable over the YTD costing process, as resulting encounter costs would capture those period-specific rates and changes.
Quarterly Costing
Calculated cost is stored for each quarter. The quarterly costing option is similar to the monthly option but computes and stores unit costs using quarterly volumes and dollars, resulting in four values of cost for each fiscal year, all stored in unique cost sets.
The differentiator for monthly vs quarterly costing is how often the team has to run cost vs the quantity of updates to the configuration for new departments, accounts, and job codes. There is also a small learning curve that occurs when only run quarterly, especially if the cost analyst is doing other work in between cycles.
Reporting implications: Similar to the monthly option, quarterly costing captures some of the cost shifts that occur during the year yet provides some smoothing of the costs like the YTD option.
Based on the frequency and approach selected, an organization will have the ability to monitor trends, exclude periods of activity, or smooth out anomalies in the cost.
LEARN MORE ABOUT HEALTHCARE AND HOSPITAL COST ACCOUNTING
301: Take Healthcare Costing to the Next Level
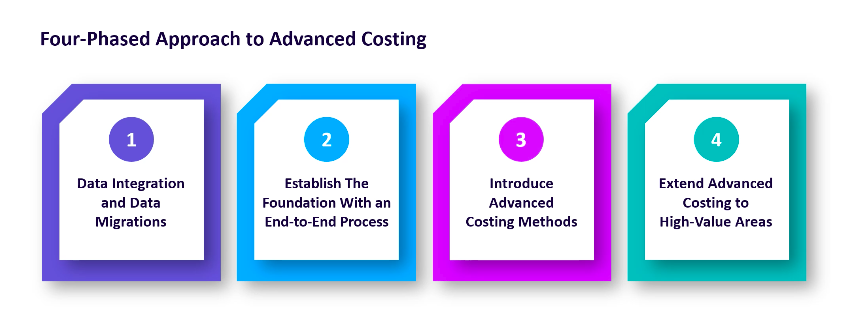
If you’re looking to evolve the cost accounting function in your organization, consider these three steps:
#1 — Get the fundamentals right
Ensure software tools are in place to streamline and fully automate the daily update of data into your decision support solution. This should include the ability to pass encounter-specific cost drivers into the model and easily reconcile against the general ledger every month. Efficient reconciliation at the general ledger and encounter level is critical to establishing buy-in around costing results, especially in large multi-entity healthcare systems.
#2 — Leverage cross-functional teams to implement changes
As new cost methods are evaluated, a cross-functional team can translate how data is captured and reflected in the care delivery process and in the various data and analytics systems. This ensures any nuances in the data are understood and accommodated early in the process, therefore increasing the credibility of costing results. In addition, frequent communication with key stakeholders will ensure that new activity codes, new payer activity, changes in strategic focus, and other drivers are accounted for ahead of time within the costing structure.
#3 — Measure twice, cut once
Don’t be afraid to try new approaches but be strategic — focus on an area where advancing the cost approach would be most impactful. Stay committed to delivering trusted results living by the motto, “Measure twice, cut once.”
Building a next-generation costing function will help organizations strengthen decision-making and optimize financial, clinical, and operational performance. But as cost inputs get larger and healthcare organizations more complex, finance leaders need platform tools that bring all costing data together and make it accessible for stakeholders to inform strategic decisions.
401: Hospital Cost Accounting Made Easy with Axiom
Axiom Cost Accounting provides healthcare leaders with an accurate, comprehensive view of performance across cost, quality, and service measures. Our costing solution supports both traditional and advanced costing methodologies and balances detail with accuracy, flexibility, efficiency, and sophistication to drive better decisions.
Within Axiom, finance teams may choose which costing method works best for their organization: RVU, RCC, RCU, Microcosting, Markup, Direct-to-Encounter, or Activity-Based.
Whether this is your first costing system, or you have a team of seasoned experts, Syntellis will be with you every step of the way — from experienced Implementation Consultants on our Professional Services team through to our Support and Optimization teams, you’re not alone on your costing journey.
You can't manage what you can't measure, so get started today with Axiom.

Partners in advanced costing
"We trusted our previous vendor to improve and update the system whenever local changes were made, but looking back at the detail that we've been able to build into Syntellis’ Axiom Cost Accounting, I’m now very aware of the number of decisions that were being made by our previous vendor without our input."

Helping you stay competitive
"If we didn’t have the core data set we have with Axiom, I don’t know how my team and I would do our job. It would be almost impossible without it.”
Modern and scalable architecture
"Axiom is so easy to use, the speed and performance of the platform make costing so much faster."
Support organization-wide decision making
"It’s really great to see your data doing what it’s supposed to do and supporting decision-making throughout the organization."
Helpful resources for healthcare cost accounting

The Journey to Advanced Cost Accounting for Better Decision-Making

Strategic Decision Support, Part 1: Next-Generation Cost Accounting
Modern Cost Accounting: Integrating Data from Healthcare Facilities and Providers

Considerations for Advanced Costing Methods in Healthcare